Diabetes has emerged as a major healthcare problem in India. According to Diabetes Atlas published by the International Diabetes Federation (IDF), there were an estimated 40 million persons with diabetes in India in 2007 and this number is predicted to rise to almost 70 million people by 2025. The countries with the largest number of diabetic people will be India, China and USA by 2030. It is estimated that every fifth person with diabetes will be an Indian. Due to these sheer numbers, the economic burden due to diabetes in India is amongst the highest in the world. The real burden of the disease is however due to its associated complications which lead to increased morbidity and mortality. WHO estimates that mortality from diabetes, heart disease and stroke costs about $210 billion in India in the year 2005. Much of the heart disease and stroke in these estimates was linked to diabetes. WHO estimates that diabetes, heart disease and stroke together will cost about $ 333.6 billion over the next 10 years in India alone.
Rapid urbanisation and industrialisation have produced advancement on the social and economic front in developing countries such as India which have resulted in dramatic lifestyle changes leading to lifestyle related diseases. The transition from a traditional to modern lifestyle, consumption of diets rich in fat and calories combined with a high level of mental stress has compounded the problem further. There are several studies from various parts of India which reveal a rising trend in the prevalence of type II diabetes in the urban areas. A National Urban Survey in 2000 observed that the prevalence of diabetes in urban India in adults was 12.1 per cent per cent. Recent data has illustrated the impact of socio-economic transition occurring in rural India. The transition has occurred in the last 15 years and the prevalence has risen from 2.4 per cent to 6.4 per cent.
The Risk Factors for Diabetes in Indians Are:
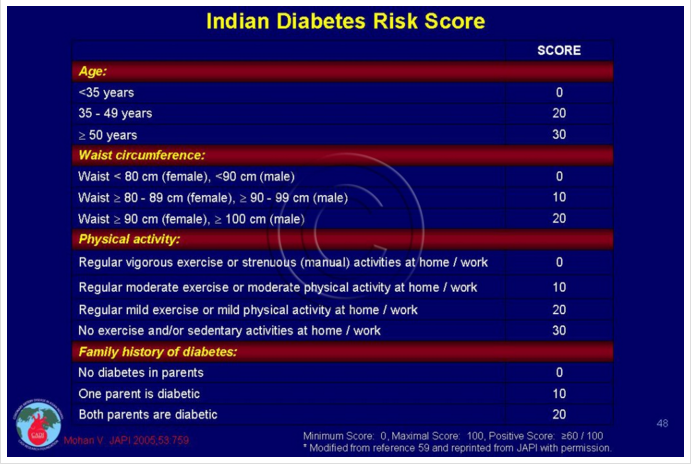
Age—Indians develop diabetes at a very young age, at least 10 to 15 years earlier than the western population. An early occurrence of diabetes gives ample time for development of the chronic complications of diabetes. The incidence of diabetes increases with age. In India, the life span has increased, hence more number of people with diabetes are being detected.
- Family History—The prevalence of diabetes increases with a family history of diabetes. The risk of a child developing diabetes with a parental history increases above 50 per cent. A high incidence of diabetes is seen among the first degree relatives. Indians have a high genetic risk for diabetes as observed in Asian Indians who have migrated to other countries. They have been found to have a higher rate of diabetes as compared to the local population .
- Central Obesity—The association of obesity with Type II Diabetes is well known. Even with an acceptable body weight range, weight gain could increase the risk of diabetes . An excess of body fat specially concentrated within the abdomen has an increased risk of diabetes. The cut-off limit for waist circumference for Indians have been recommended to be 90 cm for males and 80 cm for females. Abdominal obesity is defined by waist circumference above these limits.
- Physical Inactivity and Sedentary Living—There is enough evidence to demonstrate that physical inactivity as a independent factor for the development of type II diabetes. The availability of motorised transport and a shift in occupations combined with the plethora of television programmes has reduced the physical activity in all groups of populations.
- Insulin Resistance—Asian Indians have been found to be more insulin resistant as compared to the white population. They have a higher level of insulin to achieve the same the blood glucose control. A cluster of factors consisting of abnormal fats (Dyslipidemia), high blood pressure, obesity, and abnormal glucose levels known as metabolic syndrome is highly prevalent in Asian Indians.
- Urbanisation—The developing countries like India are undergoing rapid urbanisation . Urbanisation is associated with increasing obesity, decreasing physical activity due to changes in lifestyle, diet and a change from manual work to less physical occupations.
- Stress—The impact of stress both physical and mental along with lifestyle changes has a strong effect of increasing incidence of type II Diabetes amongst persons is a strong genetic background.
In a recent study in Chennai, nearly 25 per cent of the population studied was unaware of a condition called diabetes. Only 40 per cent of the participants felt that prevalence of diabetes was increasing and only 22 per cent of the population felt that diabetes could be prevented. Though the awareness levels increased with education, only 42.6 per cent of postgraduates and professionals including doctors knew that diabetes was preventable. The knowledge of risk factors was even lower, only 11.9 per cent of the study subjects reported obesity and physical inactivity as risk factors. Even amongst the known diabetics, only 40.6 per cent were aware that diabetes could lead to some organ damage and complications. Many people (46 per cent) with diabetes felt that it was a temporary phenomenon.
In a study in 1998, Diabcare Asia Study, it was observed that of all the patients with diabetes taking treatment from specialised centres, more than 50 per cent of patients had poor control of diabetes as per the criteria of American Diabetes Association. The Study showed that four per cent of patients were on diet therapy alone, 53.9 per cent were receiving oral antidiabetic agents, 22 per cent of the patients were taking insulin and another 19 per cent were on both insulin and oral drugs. This Study confirmed that diabetes care in India leaves much to be desired.
In two other studies carried out in Bangalore and South India, it was observed that majority of patients (70 per cent) were diagnosed by their general practitioners (GP) and 70 per cent of them had approached the GP for some other problem. 90 per cent of them underwent only Fasting and Post Meal Blood Sugar and Urine Sugar Tests. Specialised tests such as Glycosylated Haemoglobin (HbA1C), lipid profile, kidney Function test were undertaken by only four-six percent of patients. Even simple measurement of blood pressure, weight and examination of feet were not done for majority of patients.
In India, the lack of proper healthcare infrastructure, rampant ignorance and absence of clear cut guidelines mean that approach to the management of diabetes is ad hoc. The lack of awareness among patients and General Practitioners (GPs) is a key factor in the poor care. There are practically no nurse educators or diabetic counselors, no podiatrists (foot experts) and very few dieticians which means that the treating doctor has no support and has to take the entire burden of caring for these patients. The patients’ inability/unwillingness to pay for this additional support also hinders the treatment.
Even after the diagnosis, monitoring of diabetes is very poor. Most of the patients initially visit a doctor and then discontinue their therapy once their symptoms and controlled. A majority of the patients abandon modern allopathic treatment in favour of indigenous treatments. Further, more patients with poor control avoid insulin for fear of injection and belief of addiction of insulin. Hence they keep changing doctors and hop from one system of treatment to another leading to further complications and early death. Lack of resources, medical reimbursement and poor state funding for diabetes is a barrier to quality care often because the patient is unable to afford the high cost of treatment.
There is ample evidence to suggest that preventive measures to reduce the burden of diabetes are needed. The US Diabetes Prevention Programme and the Finnish Diabetes Prevention Programme and the Chinese Study have conclusively proved that lifestyle modification including weight loss, increased physical activity and dietary changes can prevent or delay the onset of diabetes. The need of the hour is direct public education and mass media campaigns, awareness about diabetes and its complications. There is a need to spread the message that diabetes is preventable and we need to have a behavioral change to adopt a healthy lifestyle.