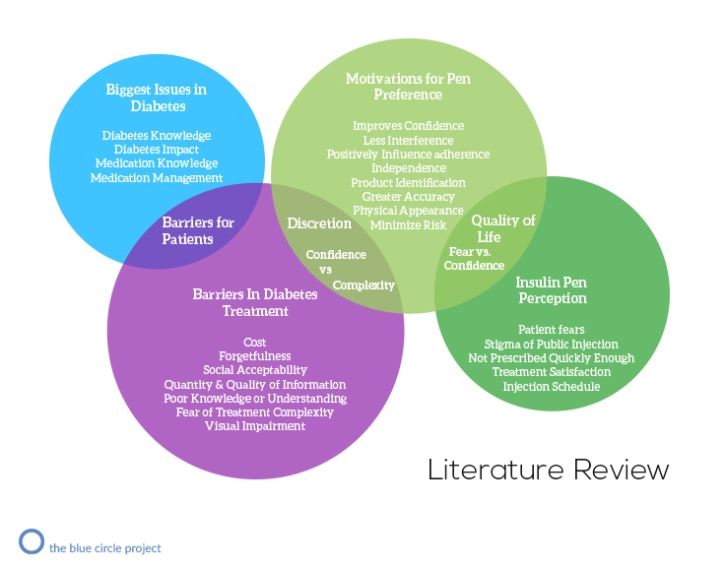
The infographic was created to condensate the information gathered from various case studies, newspaper articles and papers which represents different aspects of Diabetes Management and emotional + behavioural aspects of insulin pen users.
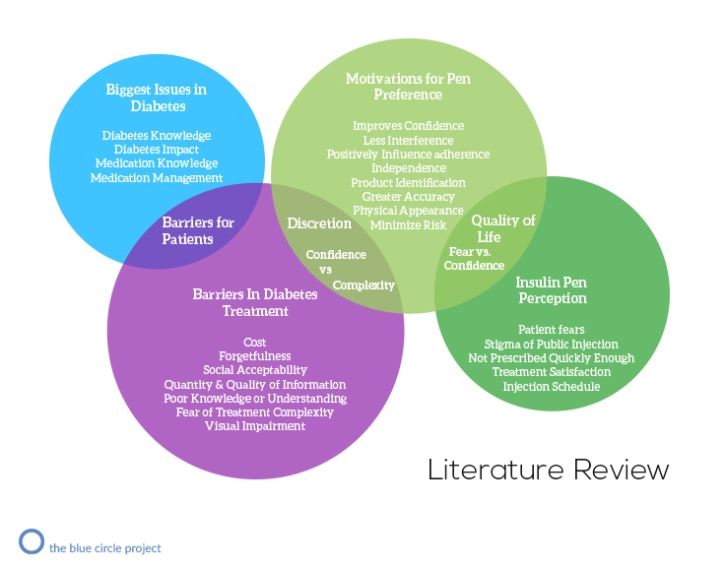
The infographic was created to condensate the information gathered from various case studies, newspaper articles and papers which represents different aspects of Diabetes Management and emotional + behavioural aspects of insulin pen users.
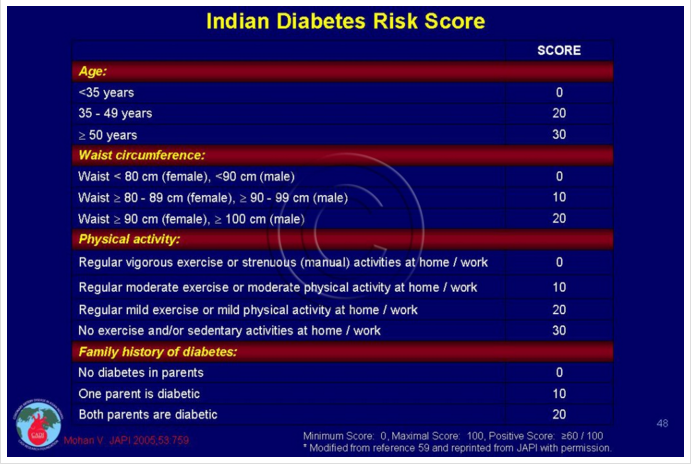
IDRS was developed using four simple parameters namely age, abdominal obesity, family history of diabetes, and physical activity. A maximum score of 100 is given for these categories combined as shown in the figure above figure. It has shown to be a highly cost effective way of testing for diabetes in a resource poor setting like India. IDRS also helps to distinguish type 2 from non-type 2 diabetes mellitus.
A Community-Based Diabetes Prevention and Management Education Program in a Rural Village in India
Research by Padmini Balagopal, PHD, CDE, RD; N. Kamalamma, PHD; Thakor G. Patel, MD, MACP; Ranjita Misra, PHD, CHES, FMALRC
This study has charted the increasing prevalence of diabetes and pre-diabetes in rural India. Educational intervention was successful in reducing some of the obesity parameters and improving dietary patterns of individuals with pre-diabetes and diabetes.
Innovative Models for the Evolving Home Health and Hospice Industry
The Visiting Nurse Associations of America (VNAA) exclusively represents nonprofit home health and hospice agencies. VNAA member agencies care for homebound patients with serious and often chronic conditions by providing a full array of health care services along with care coordination, management and prevention. Our members provide a vital link between patients, physicians and acute care settings and serve all patients without regard to their ability to pay or the severity of their illness.
VNAA members are a necessary part of the solution to improving quality and health outcomes and reducing costs in our nation’s health system.
Diabetes Prevention Through Lifestyle Change in India (D-CLIP)
The Diabetes Community Lifestyle Improvement Program (D-CLIP) aims to implement and evaluate in a controlled, randomized trial the effectiveness, cost-effectiveness, and sustainability of a culturally appropriate, low-cost, and sustainable lifestyle intervention for the prevention of type 2 diabetes mellitus in India.
Methods: D-CLIP, a translational research project adapted from the methods and curriculum developed and tested for efficacy in the Diabetes Prevention Program, utilizes innovated methods (a step-wise model of diabetes prevention with lifestyle and metformin added when needed; inclusion of individuals with isolated impaired glucose tolerance, isolated impaired fasting glucose, and both; classes team-taught by professionals and trained community educators) with the goals of increasing diabetes prevention, community acceptability, and long-term dissemination and sustainability of the program. The primary outcome is, diabetes incidence, and secondary outcomes are cost-effectiveness, changes in anthropometric measures, plasma lipids, blood pressure, blood glucose, and HbA1c, and program acceptability and sustainability assessed using a mixed methods approach.
Conclusion: D-CLIP, a low-cost, community-based, research program, addresses the key components of translational research and can be used as a model for prevention of chronic diseases in other low- and middle-income country settings.
Essential medicines list in India: Govt adds cancer, HIV, Hepatitis C and Diabetes
A good step taken by the government by subsidizing essential medicines which include pre-mix insulin 🙂
Essential medicines list in India: The Government has added 106 drugs including that of Cancer, HIV/AIDS and Hepatitis C to the list of essential medicines.
The move will ensure their availability across the country at affordable prices. This also takes the total number of items in the list to 376.
In a revision of the National List of Essential Medicines (NLEM) by the Health Ministry’s core committee, 106 medicines were added while 70 were deleted after a series of meetings and consultations across the country.
Essential medicines are those that satisfy the priority health care needs of the population. They are based on the country’s disease burden, priority health concerns, and affordability concerns etc.
The committee recommended that the list, which comes into effect immediately, be revised every three years.
Color in Medical Product Design
When considering color, you need to understand who it is that will be using the product and what will appeal to them from a color standpoint. “Appeal” doesn’t mean what colors do they like. It means what are the characteristics and values the user will associate the product with. Does your (typical) user want the product to feel precise? Intelligent? Durable? Sophisticated? Are there particular colors/color combinations that they associate with those characteristics?
David Pantalony authored an interesting article in the Canadian Medical Association Journal regarding how green became the color of hospitals and medical machines. He cites an American surgeon, Dr. Harry Sherman, as being the first to use green in the operating room in 1914. Finding the traditionally white environment to be too bright and glaring with new electric lighting systems, Sherman experimented with an operating room all in green, reasoning it was the color compliment to the red of hemoglobin. He found that his eyes could rest on anatomical features and details much better and without tiring. Around the same time, using color as a therapeutic treatment came into vogue, with green used for its calming qualities. Eventually, use of green in hospitals became pervasive.